Chapter 27 – Eleanor Lyons (D2SOP4)
Domain 2 Standard of Proficiency 4
Understand the need to empower service users to manage their well-being where possible and recognise the need to provide advice to the service user on self-treatment, where appropriate.
|
KEY TERMS Active participation Human rights-based approach Everyday practices and relationship-building Environment – emotional, cultural and structural
|
Social care is … The ability to guide and help an individual fulfil their goal with the best possible outcome. Nothing is perfect, but within social care we can help promote change and ultimately support the individual towards success in life. |
What is Empowerment?
Empowerment is a human right (Smith 2018) which is achieved through increased service user involvement, where they are supported to become independent, confident individuals in control of their own life. This chapter is written from the perspective of empowering individuals within a disability setting. Empowering any one individual brings a sense of achievement or accomplishment to the person involved. One of the many objectives as a social care worker is to empower the individual to fulfil their dreams or goals for the year. These goals may not be achievable immediately, so it the role of the social care worker to help implement a step-by-step planned process that will empower the service user to meet their needs and attain their goals in a gradual and achievable way. In the disability sector, this process is called person-centred planning.
TASK 1
How would you empower your service user to make an effective decision?
Person-centred Planning
The Health Service Executive (HSE 2018) advocates for creating empowerment cultures within health and social care settings, based on a belief that each individual should be treated with respect and dignity and should be an active participant in their own life choices and experiences. In New Directions (HSE 2018: 14) empowerment is one of the core beliefs of person-centred planning, along with equality, respect, dignity, independence, choice, inclusion and active citizenship. ‘Empowerment; person-centred planning supports the person to take control of their life. Each person is supported to have their say and their views are respected’ (HSE 2018: 14). During the course of making a care plan or a person-centred plan, the individual will work with their ‘key person’ to document what goals they would like to achieve during the course of the year.
The main aim of the person-centred plan is to get to know the service user and understand their needs and wishes for the future. Throughout the meeting, the key person and the individual will design these goals in achievable steps. This process will support the individual to successfully develop new skills based on their wishes and desires. The diagram illustrates the three themes that are discussed during the planning stage. The individual is supported to communicate what they enjoy and what hobbies and interests are part of their identity (MY SELF). MY WORLD is an opportunity for the service user to describe all the people, places and experiences that are important for them now; and MY DREAMS is all the wants and wishes they have for their short-term and long-term future. According to Sanderson (2000), the key features of person-centred-planning include active listening (in order to learn about the person), so people are encouraged to say what they want; and gathering key people together to put the plan into action. The following table, adapted from Sanderson (2000), lists what person-centred planning is and what it is not.
|
Person-centred planning is about: |
Person-centred planning is not: |
|
Listening to and learning about what people want from their lives |
The same as assessment and care planning |
|
Helping people to think about what they want now and in the future |
The same as reviews |
|
Family, friends, professionals and services working together with the person to make this happen |
Owned by services |
|
A commitment to keep learning about the person |
Just a new type of meeting |
|
For everyone who wants one |
Only for children or adults who are ‘easy to work with’ |
Different social care organisation will have alternative approaches to person-centred planning. Whatever the title used, a person-centred plan places the individual at the centre. So who attends the person-centred planning meetings? The individual will write a list of who they want to invite to the meeting, who may include a parent/guardian, sibling, family friend and any professional that works with them and is important in helping them to put this plan into action. Family and friends are partnersPlan helps build the person’s place in the communityPerson at the centrePlan reflects what is important to the personOngoing listening, learning, and further action.
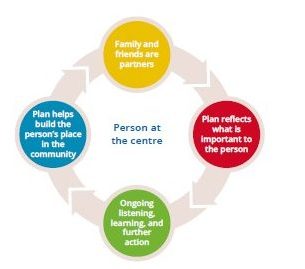
During the course of the meeting, the individual is given an opportunity to express what they want, explain how they are feeling and discuss how they want to fulfil their goals. For the non-verbal service user, creativity is used as a way of supporting them to express their goals and wishes in alternative ways. The person-centred planning process also aims to improve the service user’s self- efficacy and increase their self-confidence. Towards the end of the meeting, each individual who was invited communicates what they have understood from the meeting and shares how they can support the service user to meet their needs and achieve their goals throughout the coming year. As well as achieving goals and meeting needs, an empowerment culture (HSE 2018) can help service users gain confidence to manage their own wellbeing, where appropriate, through the support of social care workers, the staff team, family and friends.
In day services such as training centres, the staff would work towards employment for the service user to achieve independence and empower them to work in the community base. Working in the community helps the service user to feel involved and gives them a sense of belonging. To begin with, they would have someone working one-to-one with them during their working hours. Once the individual has been trained, they will continue to have a worker alongside them, to help them if they have any issues. It is important to note that the whole process of the service user attending work should be designed during their person-centred meeting. Any areas that may need improvement or what may be a concern should be highlighted and discussed, along with the supports to be provided.
TASK 2
For more information on person-centred planning, please read the HSE’s New Directions: A National Framework for Person-centred Planning in Services for Persons with a Disability (2018).
Wellbeing
The proficiency in Chapter 20 focuses on the responsibility of social care workers to take responsibility for their own health and wellbeing. In her chapter, Karen Mahon presents the WHO (2014) definition of health as including physical, mental and social wellbeing. This chapter is focused on how we can empower our service users, where appropriate, to play an active role in managing their own life and health, including their physical, mental and social wellbeing. Heslop and Hebron (2020) also adopt the WHO definition, presenting happiness as related to their view of health and wellbeing for people with an intellectual disability. This view of wellbeing acknowledges ‘a relationship between an individual and the social and environmental factors that determine their health’ (Heslop 2020: 4). Based on my practice experience this can include making the individual physically and emotionally comfortable by helping them to feel safe and loved, and promoting their good health by supporting them to make healthier choices. Other factors that can contribute to wellbeing and happiness include social contact, level of loneliness, how easy it is to get outside and be in open spaces or have opportunities to connect with people (Heslop 2020).
Working in social care, self-awareness of our own wellbeing and a knowledge of wellbeing strategies can help us to empower the individual to have a balanced outlook, to help them make healthier choices, to increase their happiness and help them through experiences such as physical or emotional trauma. As professionals, we have a duty of care to make sure the needs of the individual are met to a high standard of care and that they play an active role in managing their own health.Empowerment is only achievable through a relationship of trust developed between the service user and the worker. It is the role of the worker, through this relationship, to provide advice to the service user on strategies and ways they can improve their health and happiness. The HSE’s New Directions policy (2014) discusses consent as an ongoing process in which the service user is asked for their consent to be supported, when possible and appropriate.
TASK 3
Please read Chapter 16 on the current legislation and guidelines related to informed consent for individuals with a lack of capacity.
Consent/Self-treatment
Part of social care work is to provide advice to the service user on strategies and self-treatment options to improve their overall health and wellbeing. Guided by the HSE’s National Consent Policy (2019), when they have capacity to sufficiently understand the information and consequences of any decisions they make, their consent is needed. The individual can express their consent in writing, orally (speech) or non-verbally (nodding or hand gestures). Social care and health professionals must give the service user enough information in a way that they can understand and decide whether they do give consent. The service user’s decision must be voluntary and made without undue pressure to agree or disagree. Also, the service user must be mentally capable of communicating their decision to the social care professionals or any other health care professional, as per the Assisted Decision- Making Capacity Act 2015. This Act set out a system for adults who may have difficulties with making an important decision to have the support to make an effective choice (Inclusion Ireland 2021). In some situations, a ward of court is appointed to guide and outline consent for an individual making an important decision. The relationship between the services (health and social care) and the service users should be developed on the basis of trust and good communication. Good communication requires all parties to recognise and acknowledge the service user’s goals, their values and choices, along with guidance from the health and social care professionals (Inclusion Ireland 2021).
If the service user needs to attend treatment outside the service, the social care worker should outline to them what the appointment is for and why it is important to attend. A recent Health Information and Quality Authority (HIQA) inspection outlined the importance of the service user having a consent sheet to sign to confirm that they understand why they are at the appointment and that they can stop at any time. Before any medical treatment, such as attending hospital or the local GP, the service should ask for the service user’s consent. Depending on the situation, the service user’s next of kin or social care worker will be present at all times.
Case Study 1
John is a 35-year-old man living in a residential house in Dublin. He has mild Down syndrome and over the last year has developed a lung concern. Staff called his local GP for an appointment as John’s breathing has deteriorated. When John arrived at the appointment he refused to go in as he was not sure what the appointment was for and wanted to speak to his brother Sam. Staff explained to John the importance of the appointment and explained to Sam (John’s next of kin) that staff were concerned about John’s health. Sam asked to speak with the manager of the residential house to get a clear picture of why John did not have an explanation of the importance of the appointment before attending. The manager apologised for the lack of communication and John not being informed of the medical appointment taking place. A policy was drawn up that all residents in the house would sign the consent form and be informed about the medical appointment before attending.
Adults with intellectual disabilities, depending on their mental capacity, can orally consent and express how they feel. Children and adults with an intellectual disability could use ‘easy reads’ to help explain the appointment and help the service user to feel empowered in the process of taking responsibility of their own health and well-being. Supporting the service user to become an effective decision-maker in their own health and well-being is another important role of social care work.
So how do we empower the service user to manage their wellbeing and provide advice to the service user around self-treatment?
As social care workers we have a role, through person-centred planning, to empower the service user to build meaningful relationships, be empowered, and give informed consent. This chapter has explored the different elements that we face every day working on the frontline and dealing with the ongoing issues that the service users will face. We do not have all the answers, or the best strategies to use, but we have the ability to sit and listen to the service use and to advise them on the best actions to take.
![]() Tips for Practice Educators
Tips for Practice Educators
During the student’s time on placement, a discussion group could help ease them into their new role in the social care setting. The discussion group will help release nerves and tension and break the ice, helping all involved to build a professional relationship.
Beginning placement: At the beginning of a placement, it is important to give the student different jobs to undertake and make them feel involved in the social care setting. The jobs could be small, but this allows for casual chats between the service users and the student on placement. From here, a relationship can develop over a cup of tea or coffee, along with building common interests between the student and service user.
During placement: Once the relationships have begun to develop, the student can take on more responsibilities, based on the abilities that they have shown over the previous weeks.
- Undertaking an activities that would benefit the service user. For example, designing a wall area about what interests the service users, e.g. a television programme or music.
- Use a computer to choose colours and work out how the design will be placed on the wall. Each service user has their own part of the wall and their part of the wall will represent their own ideas.
- The wall design is a talking point for each service user to express how they see life and allow conversation to develop.
How can the social care worker guide the individual student on placement?
First, sit down with the student and get to know them over a cup of tea or coffee. This will give the student the opportunity to ask questions about the service and what their role will be for the next 12 weeks.
Outline what the social care role is within the service, what their job will be and how their role is important in empowering of the service users.
Explain that service users learn by watching the social care workers and being shown how to complete a task.
No question is a silly question – so ask the question! For example, ‘How can I help the service users manage their wellbeing and grow?’
The smallest impact can bring great achievements and empower the service user, with support, to fulfil their goals.
References
Callahan, A. M. (2013) ‘A relational model for spiritually-sensitive hospice care’, Journal of Social Work in End-of-Life and Palliative Care 9(2-3): 158-79.
Doyle, J. and Lalor, K. (2013) ‘The Social Care Practice Placement: A College Perspective’, in K. Lalor and P. Share, Applied Social Care: An Introduction for Students in Ireland, 3rd edn, pp. 151-66). Dublin: Gill and Macmillan.
Faver, C. A. (2004) ‘Relational spirituality and social caregiving’, Social Work 49(2): 241-9.
Heslop, P. and Hebron, C. (eds) (2020) Promoting the Health and Well-Being of People with Learning Disabilities. Switzerland: Springer Nature.
Heslop, P., Hebron, C., Mallett, R. and Hillman S.A. (2020) ‘Being Happy and Healthy’, in P. Heslop and C. Hebron (eds) (2020) Promoting the Health and Well-Being of People with Learning Disabilities. Switzerland: Springer Nature.
HIQA (Health Information and Quality Authority) (2021) International Review: Consent Models for Health Information (online) <https://www.hiqa.ie/reports-and-publications/health-information/ international-review-consent-models-health-information> [accessed 25 April 2021].
HSE (Health Service Executive) (2018) New Directions: A National Framework for Person-centred Planning in Services for Persons with a Disability. Dublin: National Disability Authority and HSE.
HSE (2019) National Consent Policy. Dublin: HSE.
Inclusion Ireland (2021) Assisted Decision-making (online) <https://inclusionireland.ie/assisted- decision-making/> [accessed 10 May 2021].
Mental Health Foundations (2015) What is Well-being, How can we Measure it and How can we Support People to Improve it? (online) <https://www.mentalhealth.org.uk/blog/what-wellbeing-how- can-we-measure-it-and-how-can-we-support-people-improve-it> [accessed 25 April 2021].
Sanderson, H. (2000) Person-Centred Planning: Key Features and Approaches.
Smith, S. (2018) Human Rights and Social Care: Putting Rights into Practice. Edinburgh: Dunedin Academic Press.
UKEssays (2018) Defining and Understanding Empowerment: Social Work Essay (online) <https://www.ukessays.com/essays/social-work/defining-and-understanding-empowerment-social- work-essay.php?vref=1> [Accessed 25 April 2021].
WHO (World Health Organisation) (2014) Mental Health: A State of Wellbeing. Available at <http://origin.who.int/features/factfiles/mental_health/en/> [accessed 1 May 2021).